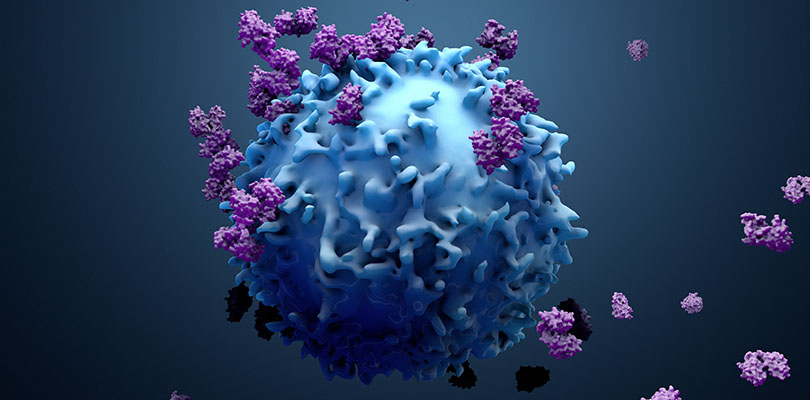
Photo Credit: simazoran / iStockPhoto.com
How Genes, Environment and Lifestyle Can Influence Your Cancer Risk
No cancer is good, but lung cancer can be particularly scary. Not only is it a “silent” cancer, bringing few if any symptoms in the beginning, but it has been known to spread far and fast. For many, a lung cancer diagnosis comes with a grim prognosis.
However, every case is different. Depending on how and why the cancer started, the outlook could be brighter. Smoking is still the biggest risk factor all across the globe, but you may be surprised to learn of the other genetic and environment variables that could work against you.
Smoking and Lung Cancer Risk
There’s no denying that smoking is the easiest way to significantly increase your risk of developing lung cancer. At least 80 percent of lung cancer deaths can be traced to smoking, and even more can be attributed to secondhand smoking.
Not every smoker will develop lung cancer. A lot depends on how and how much you smoke, along with your genetic predisposition and other factors. Doctors suspect that cancer begins when the delicate cells that line the lungs are damaged severely or repeatedly, which means your particular cancer risk rests on:
- How long you’ve smoked
- How many cigarettes you smoke a day
- When you started smoking
Above all, the length of time you’ve been a smoker is the most important factor in determining your lung cancer risk. However, the amount you smoke plays an important role, too: heavy smokers are prone to small-cell lung cancer, a type that spreads quickly and is much more difficult to treat than non-small cell lung cancer.
Tumors may be benign or malignant, and there are some important distinctions, especially when it comes to cancerous tumors.
Secondhand Smoke Can Be Just as Dangerous
Unlike smokers, people who breathe in secondhand smoke can’t quantify their intake of smoke, and that makes it difficult to pin down their specific risk of developing cancer.
However, experts suspect that people who live in a smoking house or work in a smoking environment have around a 25 percent higher lung cancer risk than those who aren’t exposed. When you spend most of your time in very smoky rooms, your lifetime risk could double.
How Can Non-Smokers Develop Lung Cancer?
Although the vast majority of lung cancer patients are long-term smokers, a healthy lifestyle won’t guarantee a cancer-free future. In fact, around 10 percent of lung cancer cases occur in people who have never smoked.
Genetic Mutations
Most of non-smokers who develop lung cancer are diagnosed with adenocarcinoma, a specific type of non-small cell lung cancer. In many cases, two gene mutations are thought to trigger this type of lung cancer in otherwise healthy people: the EGFR molecular marker and the ALK marker.
Environmental Pollution
Just as passive smokers can experience the same health complications as smokers, you don’t need to directly inhale harmful pollutants and chemicals for damage to occur. Simply living or working around these substances can raise your risk of lung cancer or mesthelioma:
- Radon gas (can rise out of the earth and seep through buildings)
- Diesel exhaust (from trucks or industry)
- Asbestos (found in older homes and buildings)
- Air pollution (heavy air pollution could be as risky as second-hand smoke)
Disease History
The illnesses you or members of your family have suffered from in the past could leave you vulnerable to lung cancer in the future. Previous lung disease (like tuberculosis) can dramatically increase your risk.
Having a first-degree relative (like a parent) with lung cancer raises your risk by up to 50 percent. However, that number could be even higher if a sibling has been diagnosed with lung cancer, and even higher if you also smoke. Experts have begun to search for a specific faulty gene to explain the family connection.
Previous Cancer
In some cases, a previous cancer can make it more likely to develop another type of cancer in the future; for many, it’s the cancer treatment that raises the risk of future problems.
Treatment for Hodgkin lymphoma, non-Hodgkin lymphoma, testicular cancer and uterine cancer will raise the risk of developing lung cancer, but not by much. If you’ve had radiation therapy for neck cancer, esophageal cancer or cervical cancer, your lung cancer risk also increases.
In some ways, lung cancer that doesn’t develop from smoking can be even more intrusive. For one, it often isn’t caught in the early stages: there aren’t many symptoms at the start, and lung cancer isn’t on a doctor’s or patient’s radar when cigarette smoking isn’t a variable.
What Research Means for Survival Rates
Lung cancer tends to get less attention than some other cancers, partly because of the smoking stigma. But without public and professional attention, less energy is put into raising awareness and funds and ultimately less money goes to research. This leave lung cancer patients — whether smokers or not — at an extra disadvantage.
However, there’s always reason to focus on the bright side. As experts learn more about genetic predisposition and gene mutations (like the EGFR and ALK markers), they can provide more targeted therapies — treatments that can add years of happy, high-quality life. Even stage four patients can have a far more optimistic prognosis than ever before.
For those who don’t have a genetic mutation, long-term survival may not be as common, but it’s also not out of reach. Taking your health into your own hands by not smoking, staying away from inhaled toxins, and knowing your family history can help you sidestep a life-threatening prognosis.